Types of infectious (septic) arthritis
There are generally two types of infectious arthritis: acute and chronic.
Acute: Caused by bacteria that begins quickly. It accounts for 95 percent of infectious arthritis. It can affect healthy people as well as people at high risk for getting an infection. Cartilage found within joints and required for normal function can become damaged within hours or days. Sometimes, infections of this caliber can occur away from the joints, in areas such as the genital organs or digestive organs, and are reactions to another infection and is called reactive arthritis.
Chronic: Begins gradually over several weeks and accounts for five percent of infectious arthritis and most often affects people who are at high risk. Most commonly infected joints include the knee, shoulder, wrist, hip, elbow, and the joints in the fingers. Most bacterial, fungal and mycobacterial infections affect only one joint or, occasionally, several joints.
Symptoms of infectious arthritis
The presentation of this condition may vary from case to case, but the following are the most commonly seen signs and symptoms:
- Severe pain that worsens with movement
- Swelling of the joint
- Warmth and redness around the joint
- Fever
- Chills
- Fatigue
- Weakness
- Decreased appetite
- Rapid heart rate (tachycardia)
- Irritability
What causes infectious arthritis?
Septic arthritis is most commonly caused by bacteria that travels through the blood stream to an area in the body. They are either staphylococcal or streptococcal.
These bacteria may enter a wound or infect the joint directly after injury or surgery. The following things that increase the chances of developing septic arthritis are:
- Joint surgery, including knee or hip replacement
- Bacterial infection elsewhere in the body
- Having a long-term condition such as diabetes or rheumatoid arthritis
- Using injected drugs
- Taking immune system suppressing medication
- Trauma and injury to the joint
Infectious arthritis risk factors and complications
Having one or a combination of these risk factors increases the chances of developing septic arthritis complications.
Existing joint problems: Chronic diseases and conditions that affect the joints, including osteoarthritis, gout, rheumatoid arthritis, or lupus. Having an artificial joint, previous joint surgery, or a joint injury can also increase risk.
Rheumatoid arthritis medications: These medications tend to suppress the immune system, creating an opportunity for infectious bacteria to invade the body and making the development of septic arthritis more likely. Also, diagnosing septic arthritis in individuals with rheumatoid arthritis is difficult because many of the symptoms and signs are very similar.
Skin fragility: Skin that breaks easily and heals poorly can give bacteria easy access. Skin conditions such as eczema and psoriasis increase the risk of septic arthritis. IV drug abusers also have a higher risk.
Weak immune system: Having an immune system that is compromised opens the possibility of becoming infected. This includes individuals with diabetes, kidney and liver problems, and those taking immunosuppressive medications.
Joint trauma: Animal bites, puncture wounds, or cuts over a joint can increase the risk of developing septic arthritis.
How to diagnose infectious arthritis?
Once at the doctor’s office, they will examine the joint for any visual abnormalities and ask you questions about the symptoms you may be experiencing.
This will only go so far in diagnosing the condition, as lab testing will be needed to find out what kind of bacteria is currently causing the infection and what medication will be the most effective. This is done by arthrocentesis—a test frequently used to diagnose this condition and involves inserting a needle into the affected area to take a sample of the synovial fluid. This fluid is then taken to a lab for testing.
The doctor may also take a blood sample, checking the white blood cell count—a marker for infection.
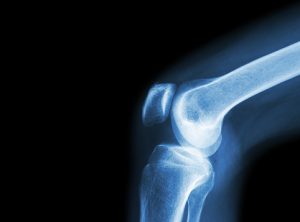
Imaging testing may also be done to assess the possible joint damage done by the infection and may include an x-ray, MRI, CT scan, or nuclear scan.
How to treat infectious arthritis?
Prescription medication
The use of antibiotics for infectious arthritis treatment is generally the most common course of action. The identification of the most likely infectious organism will dictate which is the best medication to use to fight off the particular bacteria.
Infections need to be treated promptly and aggressively to prevent osteoarthritis and damage to the joint. This may require the use of IV antibiotics, which are much more effective than their oral variants.
Synovial fluid drainage
Many people with infectious arthritis will need to have their synovial joint fluid drained. This is done to remove the infected fluid, ease the pain and swelling, and prevent further damage to the joint. Synovial fluid is often drained using arthroscopy and is done by making several small incisions near the affected joint and using a tube to suction out the fluid.
Sometimes doctors us a small needle to remove infected fluid without requiring surgery.
Other treatment options
Occasionally, surgery is required to remove any damaged sections of the joint or replace the joint altogether.
Other treatment methods to reduce pain may be used along with treatment for infection, including:
- Using nonsteroidal anti-inflammatory drugs
- Resting the joint
- Splinting the affected joint
- Going to physical therapy
Choosing to not see a doctor when experiencing the symptoms of septic arthritis can be one of the worst decisions a person can make. Losing the function of one of the larger joints on the body is simply just the start, as the infection can spread and lead to fatal consequences. When in doubt, get a doctor’s opinion to decrease septic arthritis recovery time and improve septic arthritis prognosis.
Related: Arthritis in shoulder blades, joints, and arms: Causes, symptoms, and treatment